Eosinophils are leukocytes (white cells) found in the blood and connective tissues of all vertebrates studied so far. P Ehrlich described eosinophils in 1879, although they were probably observed much earlier. Their major functions are defense against helminth parasites, allergic responses, tissue inflammation and immunity. However, is increasingly knowledge of their role in the homeostasis of tissues under remodeling processes, in both healthy and damaged tissues. Together with basophils and neutrophils, eosinophils are granulocytes (a group of leukocytes) because their cytoplasm contain many granules. The name eosinophil is because of the strong affinity for the dye eosin, which stain in pink-red the acid molecules included in these granules. In healthy conditions, eosinophils are about 2 % to 4 % of the total leukocytes of the blood. Eosinophils can exit the blood stream and move to the connective tissues of body organs, where the proportion eosinophils may be considerably higher. Curiously, eosinophils have been found in a wide variety of animals like crustacean, insects, mammals, fish, and birds, suggesting that the functions they perform have been conserved during evolution.
1. Morphology
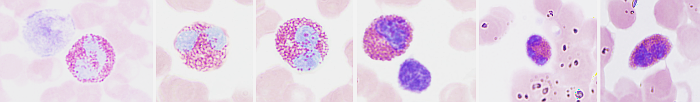
Eosinophils are rounded cells of about 15 µm in diameter, larger than other blood cells like erythrocytes, lymphocytes and basophils. At light microscopy, eosinophils show a nucleus with two lobes, and a thin nuclear bridge connecting both lobes (Figure 1). The morphology of the nucleus may change depending on the species. For example, it shows a ring-like morphology in rats. The cytoplasm contains many granules, known as specific granules, which are stained in orange-red with acidic dyes like eosin.
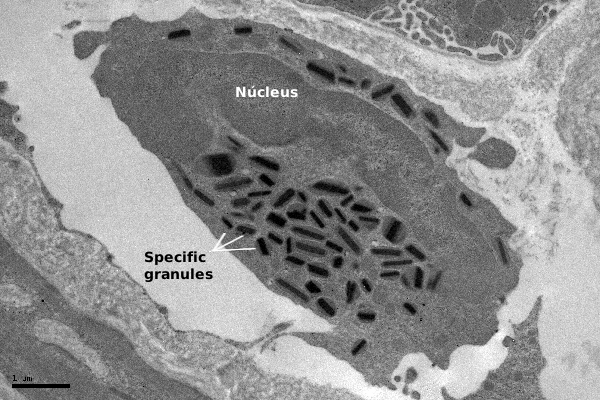
At transmission electron microscopy, the specific granules of eosinophils show a crystallized central structure arranged in parallel layers, surrounded by a more or less electron-dense matrix (Figure 2). This structure is patent in rodent, cat and human eosinophils. Furthermore, at light microscopy, a number of azurophilic granules in the cytoplasm are observed, referred to as non-specific granules. They are actually lysosomes containing acid hydrolases and other hydrolytic enzymes that contribute to eosinophil functions. In the cytoplasm, there are lipid bodies and tubule-vesicular structures known as EoSV ( eosinophil sombrero vesicles).
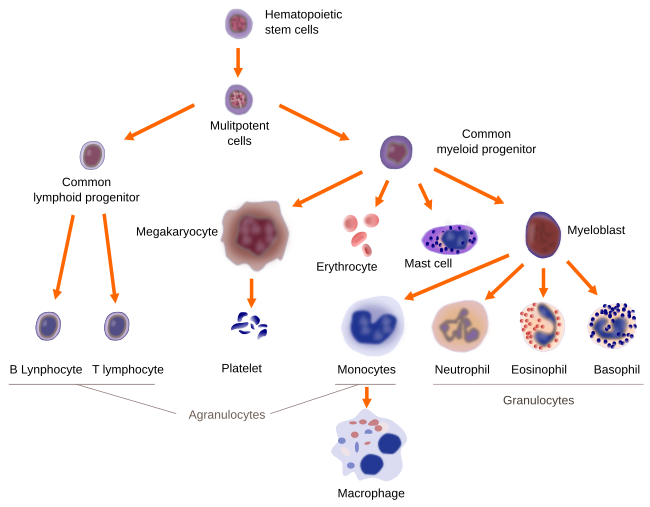
2. Origin and distribution
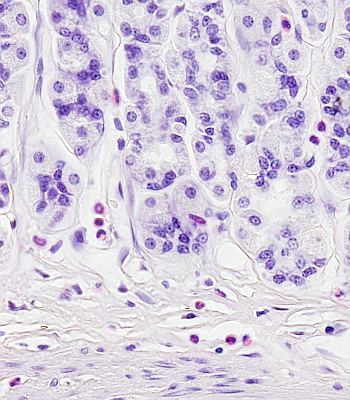
Eosinophils are originated in the bone marrow, where precursor cells of the granulocyte lineage, after 8 days of maturation, become eosinophils (Figure 3). However, by using specific cell markers, eosinophil precursors have been found in both the blood stream and in the connective tissues, meaning that not all eosinophil precursors finish their differentiation in the bone marrow. Eosinophils use the blood stream as a way to reach the final destination and perform their function. They remain in the blood for about 10 hours and then cross the endothelium of the blood vessels to go to the connective tissues, where they can live for another one or two weeks (Figure 4). Groups or a higher number of eosinophils can be found in other tissues and blood after infections. The features of circulating eosinophils are different from those found in connective tissues. For example, they can express specific cell markers depending on the tissue they are located and sometimes can be morphologically distinguished.
Recruitment
The usual number of eosinophils in normal tissues is low. However, they become more abundant when recruited by healthy tissues, developing tissues and pathological tissues, sometimes under the influence of the immune system. Thus, the number rises under some circumstances. 1) In healthy tissues with high renewing rate or with high proliferation activity of adult stem cells (small intestine, endometrial layer delimiting the uterus, bone marrow and thymus). 2) Tissues undergoing morphogenesis and development (mammary glands), in the regions where Peyer plates are formed. 3) In lungs during the postnatal development. 4) In the beige fat formation regions. 5) They are also abundant during the normal tissue repairing after damages. 6) In those tissues with intense remodeling like after infection by helmints, in lungs with acute damage, fibrosis, cancer, allergic diseases in the intestine, skin and aerial pathways. 7) In the endocrinopathies.
The high number of eosinophils in a tissue is indicative of some infection. The number of eosinophils generated in the bone marrow is low, and there are few circulating cells. During infection by helmints, allergic reactions (lung asthma, eczema, drug allergies) and other diseases, the number of eosinophils increases enormously in the blood (more than 700 eosinophils/mm3). It may happen that the number of eosinophils increases in solid tissues but not in the blood, as in the bronchial asthma, where eosinophils can be found even in the sputum.
However, it seems clear that the number of eosinophils may be increased in healthy tissues under some circumstances. These tissues share features, such as morphogenesis, cell renewing, stem cells activity and changes in the metabolic rate.
3. Functions
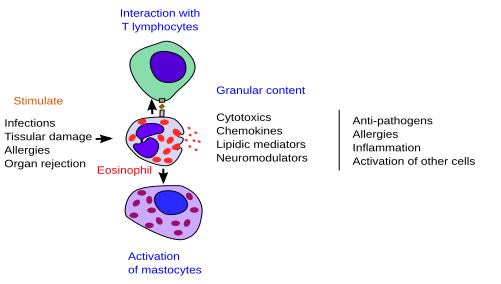
Unlike other leukocytes, the functions of eosinophils are quite variable and somehow non-precise (Figure 5). Actually, they don't look like to be necessary for the animal, since the lack of eosinophils does not have a lethal effect. It is now posed that eosinophils have similar functions in normal and pathological conditions: restore the tissular homeostasis.
Activation
The activation of eosinophils is a combined effect of antigen-presenter cells, mastocytes, T and B lymphocytes, together with all released cytokines. Three mechanisms have been described to explain the release of the eosinophil specific granule content. 1. Exocytosis. It generally happens when the eosinophil interact with a large target, such as the helmint parasites. 2. Piecemeal degranulation. This process involves the EoSV bodies (see above) that are formed in the membrane of the granules and then fuse with the plasma membrane. The formation of the EoSV bodies is started by the activation of the eosinophil, and the membrane needed is recruited from the tubular membranes of the granules. 3. Degranulation. This process is associated to the cellular lysis. It appears to be the most common mechanism and would explain the presence of many eosinophil granules in tissues under inflammation processes produced by helmints and allergic responses.
Action
The functions of eosinophils depend on the substances stored in the granules. There are four main proteins: the mayor basic protein (MBP) is enriched in arginine, provides acidophilia and is located in the crystal structure, the eosinophilic cationic protein (ECP), the eosinophil peroxidase (EPO) and the eosinophil derived neurotoxin (EDN). They are no exclusive of eosinophils, since MBP and EPO are found in basophils, and EDN and ECP are found in neutrophils. These and other molecules stored in the granules make possible a very fast response (less than one hour).
All molecules mentioned above show activity against parasites because they are cytotoxic and contribute to the destruction of pathogens. For example, eosinophils are able to get attached to other cells and kill them thanks to their cationic proteins that form pores in the membrane of the pathogen cell. These pores are the entry way to other molecules that definitely kill the cell. However, these proteins have other non-toxic functions since they are involved in adaptive and innate immunity by interactions with T lymphocytes and mastocytes.
Specific granules also contain enzymes like histaminases and arylsulphatase, which are involved in inflammation after allergy processes. They contribute to neutralize the effects of histamine released by mastocytes and leukotrienes released by basophils.
There is an increase of eosinophils during asthmatic processes related to the inflammation that happens in this disease. Eosinophils may produce a worsening of the disease. This is because they may release more than 35 different cytokines, chemokines and growth factors. At least 10 of these molecules are stored in the granules as preformed molecules, mainly around the crystalloid. Other molecules, however, are stored in small vesicles. The ability of eosinophils to synthesize and release a large variety of active molecules means that they are involved in many functions. Eosinophils may also perform several immune roles, such as presenting antigens and favor the inflammatory response.
Other functions performed by eosinophils are involved in the normal functioning of some organs. For example, there are waves of eosinophils in the endometrium that correlates with the hormones cycles, which are thought to be related with a reproductive activity. They are also abundant in mammary glands during the postnatal period, and it is thought that they may help with the normal development of these glands. In the thymus, there are also perinatal waves of eosinophils that appear to be important for removing thymocytes by apoptosis.
Thus, it is thought that eosinophils are cells performing functions to recover tissular homeostasis, as well as participating in normal renewing and cellular proliferation of tissues.
-
Bibliography ↷
-
Davoine F, Lacy P. 2014. Eosinophil cytokines, chemokines, and growth factors: emerging roles in immunity. Frontiers in immunology 10. doi:10.3389/fimmu.2014.00570.
Muniz VS, Weller PF, Neves JS. 2012. Eosinophil crystalloid granules: structure, function, and beyond. J Leukoc Biol. 92:281-288.
Padigel UM, Nolan TJ, Schad GA, Abraham D. 2006. Eosinophils can function as antigen-presenting cells to induce primary and secondary immune responses to Strongyloides stercoralis. Infection and immunity. 74(6): 3232–3238.
Rothenberg ME, Hogan SP. 2006. The eosinophil. Annual review of immunology. 6. 24:147-174.
-