1. Sight
2. Hear
3. Taste
4. Smell
5. Skin senses
6. Blood pressure
In this page, we are going to deal with structures and systems responsible for fetching information coming from both the outside and inside the animal body. These systems are commonly known as senses. Although we will also deal with them in other pages related to other animal organs, a more detailed description is given here. The senses that get information from the environment are sight, hearing, smell, taste, and touch. Other tissular structures process the inner physiological state of the body, such as pain, temperature, body balance, and blood pressure.
1. Sight
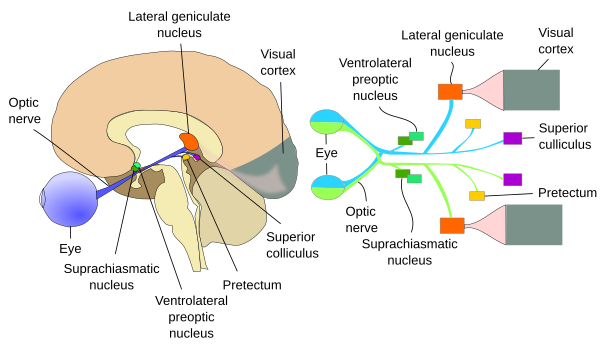
In vertebrates, the eye is the sensory organ for detecting visible light. It is an ovoid structure made up of several tissue layers that are able to project and focus the light onto a layer of neurons, the retina. The retina transforms the light into nerve impulses that travel through the optic nerve (cranial nerve II) to the thalamic geniculate nucleus and other encephalic structures. In the occipital lobe of the encephalon, the visual information reaches the visual cortex through axonal projections from the geniculate nucleus (Figure 1).
Eye
The eye is the structure that detects the light reflected by objects and transduces it into electrical information, which, after local processing, is sent to other parts of the encephalon for interpretation. Eyes are rounded and polarized structures. From the anterior to the posterior part, they are made up of the cornea, anterior chamber, iris, ciliary muscles, crystalline, vitreous body, retina, choroid, sclerotic, or sclera, and optic nerve. These components are distributed in three concentric layers or tunics (excepting the crystalline): fibrous tunic, vascular tunic, and internal nervous tunic (Figure 2).

The cornea is the most external part of the eye, so it is in contact with the air (Figure 3). It is a transparent structure that focuses the light and protects the eye surface. The optic properties of the cornea are a consequence of the arrangement and type of collagen fibers it contains. There are no blood vessels in the cornea, and that is why it is relatively easy to transplant this part of the eye during surgeries.
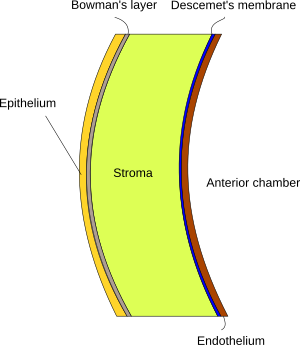
The cornea is a sheet of tissue made up of five layers: corneal epithelium, Bowman's layer, stroma, Descemet's membrane, and endothelium (Figure 2). The corneal epithelium is the outer layer. It is a stratified squamous epithelium containing many nervous fibers, and it can be easily auto-repaired. The corneal epithelium is laterally continuous with the epithelium of the conjunctiva. The Bowman's layer is found immediately beneath the corneal epithelium. This layer is not found in all mammal species. Bowman's layer contains collagen fibers but not elastic fibers. The stroma, found under the Bowman's layer, is the thicker layer, accounting for about 90 % of the thickness of the cornea. The stroma is connective tissue with collagen fibers, mainly types I and IV, arranged in layers with different spatial orientations of the fibers between adjoining layers. There are also proteoglycans like chondroitin sulfate and keratan sulfate. Some cells are also present, such as fibroblasts and errant lymphocytes. Descemet's membrane lines the inner part of the stroma, and, actually, it is the basal lamina of the endothelium that follows. The endothelium is the innermost layer of the cornea and forms the anterior wall of the anterior chamber of the eye. The cornea is laterally connected with the sclera through a region known as the corneal limbus.
The ciliary body is found behind the iris and performs two main functions: release vitreous humor and change the shape of the crystalline to focus the light on the retina. It links the ora serrata of the choroid to the root of the iris, and it is connected to the crystalline by a ligament. The ciliary body shows a ring shape and, in transverse sections, looks like a triangle (Figure 4). It is divided into two components: pars plicata and pars plana. Pars plicata is found close to the crystalline lens, and it is organized in finger-like structures known as ciliary processes, whereas pars plana shows a flattened form. The smooth muscle of the ciliary body is known as the ciliary muscle, which controls accommodation by changing the shape of the crystalline lens to focus the light on the retina. The internal part of the ciliary body is dense connective tissue with abundant elastic fibers and blood vessels. The ciliary epithelium is made up of two layers. The most internal one is pigmented and releases aqueous humor. The ciliary body, together with the iris and choroid, constitutes the uvea, or vascular tunica.

The iris is the structure of the eye that separates the anterior chamber from the posterior chamber, and it is attached to the ciliary body through its peripheral region. In the central area of the iris, there is an opening known as the pupil, through which light can reach the crystalline lens. The pupil area of the iris is the closest part to the pupil, and the peripheral part is known as the ciliary area. The iris is highly vascularized, loose connective tissue. No matter the diameter, blood vessels show the same organization. They do not contain a muscle layer. The posterior part, the deepest one, of the iris is a two-layered, highly pigmented epithelium, which gives color to the eyes depending on the amount and arrangement of the pigment. The iris works as an adjustable diaphragm thanks to the activity of two muscles. One of them is the sphincter of the pupil, which sets the diameter of the pupil. It is smooth muscle innervated by parasympathetic fibers of the ciliary ganglion and is arranged circularly. The other muscle is the dilator muscle, which increases the pupil's diameter (pupil dilation). It is composed of radially oriented myoepithelial muscle cells, which are innervated by sympathetic neurons of the superior cervical ganglion.

The crystalline lens is located behind the pupil and shows a transparent biconvex body. Covering the crystalline, there is a transparent, thick external layer known as the capsule, which contains a similar molecular composition to the basal lamina of other tissues. Below the capsule, in the superficial part of the crystalline lens, there is a one-cell-thick layer of cuboidal cells that is not present in the peripheral parts. Besides these cuboidal cells, most of the crystalline lens is made up of cells known as crystalline fibers because they are very long, up to 10 mm, but very thin, a few µm. These cells contain a high concentration of the protein crystalline, which accounts for almost 90 % of the total protein content of the crystalline lens and is responsible for the optical features. The cornea and crystalline lens work together to focus the light on the retina. The crystalline lens can be stretched by the muscles of the ciliary body, changing the curvature and thus the focusing properties. In addition, its position depends on ciliary fibers.
The vitreous body fills the cavity between the crystalline lens and the retina. It is a gelatinous substance with similar transparency to crystal glass and composed of an aqueous solution with abundant type II and XI collagen and hyaluronan. It also contains some scattered cells known as hyalocytes.
The retina is the light-sensing structure of the eye and the innermost tunica of the eye. It results from an evagination of the central nervous system during embryonic development. This evagination folds to get a cup-shaped morphology with two layers: a pigmented external one and a nervous internal one, which is the retina. The retina is composed of several types of neurons: those that convert light into electrochemical gradients (that is, photoreceptors), neurons that receive and process the information from photoreceptors, and neurons that send the processed information through the optic nerve to the encephalon. There are up to 10 layers of neurons in the retina (Figure 6). The most external one is the photoreceptor layer, which has two types of photoreceptors: cones and rods. Cones are specialized in perceiving colors, whereas rods respond to light intensity. Cones are more abundant in the fovea, an area of the retina where the eye focuses the light. When we rotate the eyes to see an object, we are actually moving the fovea to receive the focused light coming from the object we are interested in. The axons of the optic nerve arise from neurons located in the innermost layer of the retina, the ganglionar layer. That is why these axons must cross the photoreceptor layer, leaving a spot without photoreceptors, which is then a blind spot. We are not aware of this blind spot because our encephalon "fills" for us. The pigment layer is the outermost layer that results from the evagination and does not contain neurons but pigment cells. The pigments prevents light dispersion, contributing to more sharp vision. This layer is in close contact with the photoreceptor layer and is also involved in the homeostasis of photoreceptors.

2. Hearing
The auditory system is in charge of auditory perception. It actually consists of two subsystems: auditory and vestibular. The auditory component perceives sounds and transduces them into electrical signals. The vestibular component maintains the balance of the body and spatial orientation. The auditory system is spatially divided into three components: the external ear, the middle ear, and the inner ear (Figure 7).

Outer ear
The outer ear is composed of the auricle (pinna) and the auditory canal, which communicates the external environment with the tympanic membrane or eardrum. The auricle is usually oval and mostly made up of elastic cartilage and integument (skin). It is delimited by a thin epidermis and many hair follicles, though it depends on the animal species. The auditory canal is a long, tube-like structure that starts in the auricle and ends in the tympanic membrane. The outer part contains many glands, known as ceruminous glands, that release lipidic components. These substances get mixed with the secretion of the sebaceous glands, forming the earwax, or cerumen. The internal part of the auditory canal gets inside the cranial bone, and both types of glands progressively disappear.
Middle ear
The middle ear is found after the auditory canal. It is a cavity, known as the tympanic cavity, inside the cranial temporal bone. The tympanic membrane separates the auditory canal from the tympanic cavity. Inside the tympanic cavity, there are three tiny bones (ossicles): the malleus, the incus, and the stapes, and the muscles that move them (Figure 8). The Eustachian tube is also part of the middle ear and connects the tympanic cavity with the pharynx. This connection allows for a balance between the air pressure of the oral cavity (atmospheric pressure) and that of the tympanic cavity. The middle ear is separated from the inner ear by the bony inner medial wall.

The function of the middle ear is to transform the air waves, which carry sound information, into mechanical movements of the ossicles, which convey information to the inner ear. The process begins with the pressure of the air waves coming through the auditory canal on the tympanic membrane. Vibrations of the tympanic membrane move the ossicles of the middle ear: first the malleus ossicle, which is in contact with the tympanic membrane, second the incus, and third the stapes. The stapes transfers the information to the labyrinth of the inner ear (see below), where it creates currents. The communication between the stapes and the labyrinth is through the oval window (fenestra vestibuli) and round window (fenestra cochleae) of the bone. In the tympanic cavity, there are two muscles, one attached to the malleus and the other to the stapes. The malleus keeps the tympanic membrane stretched, and the stapes compensates the movement of the incus. Both muscles are important for alleviating the higher vibrations and protecting against very loud sounds.
Inner ear
The inner ear is the labyrinth (Figure 9). There are two parts: the bony labyrinth and the membranous labyrinth. The bony labyrinth is inside the temporal cranial bone and comprises the semicircular canals, vestibule, and cochlea. The vestibule is in the center of the bony labyrinth, and the semicircular canals are connected with the vestibule by both of their ends. There are three semicircular canals inside the bone: superior, posterior, and lateral. The inner cavity of the canals is continuous with the cavity of the vestibule. On the other side, the vestibule is connected with the cochlea, which is a spiral-shaped conduct.

The membranous labyrinth is located within the cavity of the bony labyrinth. In the vestibule, there are two compartments: the utricule and the saccule. The utricule cavity is connected with the cavities of the membranous labyrinth, with its membrane lining the internal surface of the semicircular canals. The utricule plus membranous semicircular conducts form the vestibular labyrinth. The saccule is connected with the cochlear canal, which extends through the interior of the cochlea. The saccule and cochlear canal form the cochlear labyrinth. All these cavities are filled with the liquid substance endolymph. On the other hand, the perilymph fills the vestibular and tympanic canals of the cochlea.
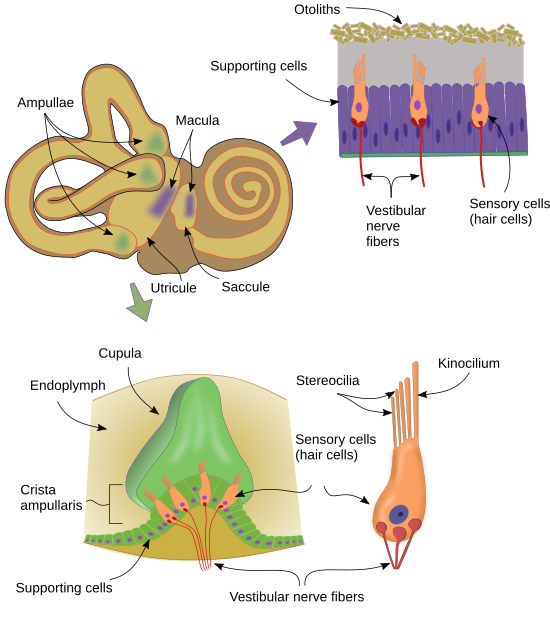
Some regions of the labyrinth contain receptor cells that can sense the change in body speed, position, and the sound (organ of Corti by means of the ossicles of the middle ear) (Figure 10). These cells transform the changes in the movement of the liquid around them (endolymph) into electrical signals. The transduction is done by cellular apical structures known as stereocilia, which are actually modified microvellosities, and by real cilia known as kinocilia. In the ampullary crests, located between the semicircular canals and the utricule, the receptor cells (hair cells) sense angular movements of the head thanks to the bending of the stereocilia and kinocilia pushed by the current of the endolymph and convert the mechanical inputs into electrical information. In the saccule and utricule, there are also receptors that can sense gravity (the vertical or horizontal position of the body) as well as lineal speed changes.
The organ of Corti is found in the cochlear canal, more precisely in the scala media (Figure 11). It is composed of an epithelial layer containing ciliated cells. The movements of the inner ear ossicles are converted into endolymph streams, which bend the cilia and kinocilia and generate the electrochemical gradients that carry the sound information.

The inner ear is innervated by the vestibular nerve (VIII). This nerve is divided into two branches: vestibular and cochlear. The vestibular branch innervates the cell receptors of the labyrinth and vestibule, whereas the cochlear branch innervates the auditory receptors. Vestibular nerves have their neuronal soma in the vestibular ganglia (there are two), which are located outside the labyrinth. The ganglion of Corti, or spiral ganglion, forms the cochlear branch and is located in the cochlea.
3. Taste
The gustatory sense recognizes dissolved molecules that enter the mouth, normally food. However, the taste of food depends mostly on smelling, i.e., the olfactory sense. The structures responsible for perceiving gustatory information are the gustatory buttons, which mostly localize in the tongue papillae, but they can also be found in other locations of the oral cavity. Papillae are protrusions of the tongue surface and are named according to their morphology: filiform, fungiform, foliate, and calyciform. Gustatory buttons are found on the tips of the fungiform papillae and in the lateral and deep walls of the calyciform papillae.
The gustatory receptor cells are found in the gustatory buttons. These receptors make synaptic contacts with primary sensory axons, which enter the encephalon through the IX and VII cranial nerves. They innervate the nucleus of the solitary tract, which in turn sends axons to several thalamic nuclei. From the thalamus, gustatory information is sent to the gustatory cortex.
Tongue
Tongue is the organ where papillae wiht most of the gustatory buttons are locted. Briefly, the tongue is a striate skeletal muscle inside the oral cavity that moves food, and helps to shape sounds emited by some animals.
Gustatory buttons are structures that recognize molecules responsible for taste. They are found in the tongue papillae and in other locations of the oral cavity, such as the palate and epiglottis. The cells of gustatory buttons are organized like an onion (without leaves), with the apical part in contact with the external surface (Figure 12). There are three cellular types: support, neuroepithelial, and basal cells. Support or subtentacular cells are located at the periphery of the gustatory button. Neuroepithelial cells are found more inner. There are about 10 to 14 neuroepithelial cells per gustatory button. These cells are the receptors that recognize taste molecules and transduce the information into signals that are transmitted to nerve terminals. These nerve terminals are in close apposition to the membrane of neuroepithelial cells. The basal cells, the third type, are located basally and at the periphery of the gustatory button, in contact with the basal lamina. Basal cells have been proposed to be stem cells that are able to divide, differentiate, and replace the cells that die during normal renewal of the gustatory button cell population.

The information produced by receptor cells of the gustatory buttons, after they recognize taste molecules, is gathered by different nerves depending on the zone of the tongue where gustatory buttons are located (Figure 13). Those at the anterior part (close to the tip) and medially are innervated by the facial nerve (VII), the posterior part of the tongue and the pharynx epithelium are innervated by the glosopharyngeal nerve (IX), and the larynx and epiglottis are innervated by the vagus nerve (X). Although these nerves enter the rhombencephalon at different levels, the information converges at the rhombencephalic nucleus of the solitary tract, and then it is sent to the thalamic centers, which send axons to the gustatory cortex. There are other lateral pathways and outputs from the gustatory cortex that associate the gustatory information with the rest of the relevant information for the organism. For instance, taste is a mix of gustatory information and smell information, i.e., two different types of information coming from different receptors and different nervous pathways and processed separately should be integrated.

4. Olfaction
Olfaction, the sense of smell, is probably the most ancient of the senses. It is involved in feeding, social communication, predation behavior, spatial orientation, offspring care, parental imprinting, and so on. The high relevance of this sense is clearly shown when the olfaction system is damaged. In rats, it causes changes in sleeping patterns and sexual behavior, increases aggressiveness, and leads to poor care for progeny and anxiety. The basic components of the olfactory system have been conserved during evolution for millions of years. It is of interest that insects show a similar basic molecular mechanism for olfaction as vertebrates, and the first cellular components of the olfactory system are similar.
The olfaction process begins in the olfactory epithelium, located in the deeper part of the nasal cavity, close to the cranial bone (Figure 14). The olfactory epithelium contains neurons (olfactory receptor neurons) with transmembrane receptors that recognize olfactory molecules. These neurons have axons that form the olfactory nerve (nerve I), which crosses the cranial bone through the so-called cribriform plate and enters the olfactory bulb, the most rostral part of the encephalon. The axons of the olfactory nerve divide into fascicles, and their ends form round nets known as olfactory glomeruli. In each glomerulus, the primary olfactory information is transmitted to other neurons, mainly mitral cells. From the olfactory bulb, the olfactory information is sent to other deep encephalic areas, where it is processed and confronted with other types of information. For instance, the smell of food has not the same impact on the behavior of the animal when it is hungry as when it is satiated.

Olfactory receptor neurons in the nasal cavity are distributed in different groups. Most of them are found in the main olfactory epithelium, close to the cribriform plate. Other olfactory receptor neurons are found in the vomeronasal organ, which in humans is located in a bone cavity of the septum at the base of the nasal cavity. However, fish lack the vomeronasal organ. In non-human vertebrates, there are other olfactory structures, like the septal organ of Masera and the organ of Grueneberg (Figure 15). It is thought that each of these structures senses different olfactory information.

Main olfactory epithelium
The main olfactory epithelium is pseudostratified, made up of several types of cells, and is about 1 cm2 in humans. The main cell type is the olfactory receptor neuron, which recognizes the olfactory molecules and then produces an electric response by depolarization. These neurons are bipolar with an apical (free) membrane with cilia or microvilli, where the transmembrane olfactory receptors are located. Each receptor neuron expresses only one type of transmembrane olfactory receptor, and there are thousands of different transmembrane olfactory receptors. Thus, in the main olfactory epithelium, there are thousands of olfactory receptor neuron populations that are able to sense a particular and different olfactory signal. At their basal domain, the olfactory receptor neurons have an axon that leaves the main olfactory epithelium, joins other olfactory axons, and they together crosse the cribiform plate on their way to the olfactory bulb. Interpersed with olfactory receptor neurons, there are the supporting or subtentacular cells, which are involved in supporting and, likely, in the electrical isolation of the olfactory receptor neurons. Another cell type forms the Bowman's glands, that synthesize and release mucous substances that cover the outer surface of the epithelium. Finally, at the basal part of the main olfactory epithelium, there are the basal cells. The function of the basal cells is to proliferate and replace the other cell types of the epithelium. This is one salient feature of the olfactory epithelium: a permanent turnover, where the cells die and are replaced by new ones.

5. Skin senses
The skin, the largest sensory organ of the body, has several types of receptors that get information from the external environment: mechanical (touch, pressure, vibration), temperature, and pain receptors (mechanical and chemical damages). Unlike other senses that gather the receptors in an organ, cutaneous receptors are scattered through the skin of the body as either free or encapsulated nerve endings. Different parts of the body show different receptor densities. The sensory mechanism of these receptors is similar: a sensory input changes the shape or directly affects the nerve membrane so that the electrochemical membrane potential is modified, and this is transformed into an action potential that travels via nerve fibers to neuronal bodies. From the neuronal body, the information is sent to the central nervous system.
Cutaneous receptors can be classified regarding their location, type of stimulus they are responding to, or how their nerve endings are organized.
Free nerve endings. They are the naked final ends of the nerves, not wrapped with myelin (myelinization stops before these final segments), nor with any other structure. They can be mechanoreceptors (touch), nociceptors (pain), or thermoreceptors (temperature). They are distributed in both the epidermis and dermis.
Free nerve endings may be associated with particular types of cells (Figure 17). For instance, Merkel disks are cup-shaped free endings that partially coat the Merkel cells of the epidermis. Merkel disks are mechanoreceptors with high sensitivity and slow adaptation to the stimulus, so they can inform about long-lasting stimuli. They are abundant in the fingertips and lips, although they are also found scattered in the skin of other parts of the body. There are other free nerve endings, known as peritrichial endings, around the hair follicles. Peritrichial endings are mechanoreceptors usually showing a fast adaptation to the stimulus, i.e., they respond to changes in the stimulus, even slight changes, but not to a sustained stimulus.

Receptors involved in pain transmission are very thin and stimulated by molecules released by damaged cells. Analgesics work to avoid this activation at different levels, depending on the drug.
Encapsulated receptors. The nerve endings are wrapped by other cells in the encapsulated receptors, commonly connective tissue cells, which are arranged as onion leaves. Most of these receptors are mechanoreceptors, although some are thermoreceptors, and they are more often found in the dermis.
Meissner's corpuscules. They are encapsulated receptors found in the dermis, usually in the dermal papillae of the skin lacking hair follicles. The capsule is made up of several layers of connective tissue, and the nerve endings are twisted among these layers. A mechanical input causes the layers to be separated from each other, triggering a change in the membrane of the nerve. These receptors show slow adaptation, so that even if the stimulus persists, the transmission of the information stops. This ability is very useful to discern the movement of objects over the skin, but forget about them if they stay quiet. Meissner's receptors are so sensitive that the brain can discern the spatial direction of the movement or the texture of the object. They are abundant at the fingertips and lips. Those located in the skin of genitals and nipples are known as the genital's corpuscles.
Pacinian corpuscles. They are encapsulated receptors found in the deep dermis, pleura, nipples, pancreas, tendons, penis, and clitoris, as well as in more internal locations like the urinary bladder and joints. They are stimulated by fast movements like vibrations and by strong pressure forces. The size and morphology of Pacinian corpuscles are variable, and it looks like the deeper the location, the larger they are. Golgi-Mazzoni corpuscles show similar organization to the Pacinian corpuscles, but they are more simple and mainly located at the fingertips.
Ruffini corpuscles. They are encapsulated receptors found deep in the skin. They show slow adaptation, so they respond to long-lasting stimuli. These receptors are also found in the joint capsules, where they process information about the rotation of the bones. Besides mechanical stimulus, they can also sense temperature and pain.
Krause corpuscles. They are encapsulated receptors found in the dermis and oral cavity, where they sense pressure and temperature. They show fast adaptation.
6. Blood pressure
Blood pressure is controlled by the so-called baroreceptor reflex. It is very efficient and keeps the blood pressure within a tight range of values. The baroreceptor reflex consists of an afferent component that brings information about the state of the blood pressure to the central nervous system and an efferent component that affects the mechanisms that change the blood pressure.
The afferent component consists of nerve terminals known as baroreceptors. These are mechanoreceptors found in the walls of the blood vessels and heart and are stimulated when the walls are stretched. There are high-pressure baroreceptors and low-pressure baroreceptors. High-pressure barorecepros are located in the carotid sinus and in the aortic arcs, while low-pressure baroreceptors are found in the atrium and heart ventricles, as well as in the lung veins.
The nerves that carry the blood pressure information of the aortic arches and carotid sinus enter the encephalon through the vagus (X) and glossopharyngeal (IX) nerves, respectively. This information reaches the nucleus of the solitary tract of the rhombencephalon. Then, the processed information is sent through the efferent component (autonomous nervous system) and modifies the muscle contraction of the blood vessels and heartbeat rhythm.
The activation of baroreceptors also induces the release of vasopressin (an antidiuretic hormone) by the hypothalamus, leading to a thirsty sensation, and the release of renin by the kidney, modifying vasoconstriction (mediated by angiotensin II), sodium reabsorption, and so on.
 Peripheral nervous system
Peripheral nervous system