1. Features
- Cell types
- Matrix
2. Trabecular bone
3. Compact bone
4. Osteogenesis
- Intramembranous
- Endochondral
Bone tissue, together with the bone marrow and other connective tissues, forms the bones, which have a twofold function: mechanical support and metabolic center. Bones support the soft parts of the body and protect organs like the brain, lungs and heart. They also work as a lever used by muscle to produce movement. As a metabolic center, bones store calcium and phosphorous, and regulate their metabolism. In addition, in the internal cavities of bones, the bone marrow is made up of many stem cells (hematopoietic cells) that differentiate into blood cells, a process referred as hemaotopoiesis.
1. Features
The features of the bone tissue depend on the cell types and the extracellular matrix they are made up of.
Cell types

Osteoblasts are cells specialized in synthesizing bone extracellular matrix, and responsible for bone growth and remodeling. They are found in the growing surface of the bone, lined up in a somehow layer of about one cell in thickness. This initial bone matrix, called osteoid, is no mineralized yet. Osteoid matures by precipitation of calcium salts. When osteblast are completely surrounded by extracellular matrix, they are confined in a cavity known as bone lacunae and then differentiate in osteocytes, the mature bone cells.
Osteocytes are the most abundant cell type in the mature bone. They are locked in extracellular matrix cavities (bone lacunae), and look like spiders with long legs. These "legs" are cytoplasmic extensions inside extracellular matrix tunnels or bone canaliculi (see compact bone). Through these extensions, osteocytes can exchange substances between each other and reach the blood vessels. Many molecules do not easily diffuse through the mineralized bone extracellular matrix. Osteocytes maintain the extracellular matrix by both synthesis and reabsorption of its components. They are also involved in the calcium metabolism and in the homeostasis of this ion in the body by releasing calcium from the extracellular matrix.
Osteoclasts are the cells that degrade and remove bone, both mineralized and organic extracellular matrix, by a process known as reabsorption. Osteoclasts are multinucleated and very large cells.
Bone extracellular matrix
The most characteristic component of bone tissue is the mineralized extracellular matrix containing hydroxyapatite minerals (crystallized calcium phosphate is up to 65% of the bone extracellular matrix). The remaining of the extracellular matrix is composed of organic molecules, including highly abundant collagen fibers and smaller amounts of glycosaminoglycans. Extracellular matrix allows the bone tissue to show great consistency, hardness, compression strength, and some elasticity. Unlike cartilage, bone tissue is heavily irrigated by the blood system.
Depending on the density of the extracellular matrix, two types of bone tissue can be distinguished: a) cancellous or trabecular bone, when the bone tissue has large spaces that give a loose or spongy appearance; b) compact or cortical bone, when the extracellular matrix is very dense and empty cavities are not found (Figure 1).
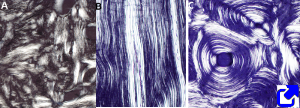
At light microscopy, there are three categories of bone tissue depending on the collagen fiber organization: non-laminar (interwoven collagen fibers), laminar (paralell collagen fibers associated in bundles), and osteonic or concentric laminar (collagen fibers forming concentric rings) (Figure 1).
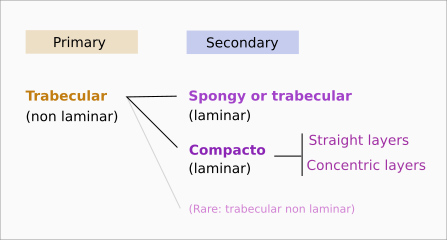
2. Trabecular bone
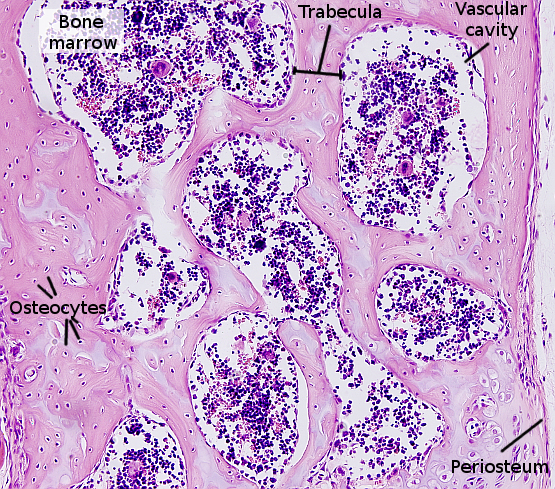
Trabecular or spongy bone (Figure 2) has large inner spaces known as vascular cavities. These cavities are occupied by blood vessels and hematopoietic cells. Bone trabeculae are the walls of vascular cavities. Trabeculae contain collagen fibers arranged in lamellae (lamellar trabecular bone) or, more rarely, intertwined collagen fibers (woven trabecular bone). Generally, during the formation of bone, i.e. osteogenesis, the woven trabecular bone is first formed, which is called primary bone (Figure 1). It is subsequently replaced by a secondary bone, which is mostly laminar bone. There are two types of secondary bone: compact and trabecular bones.
3. Compact bone
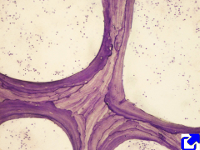
Compact or cortical bone has no vascular cavities, and the extracellular matrix is organized into bone lamellae, which can be arranged straight and parallel (lamellar compact bone) or concentrically around a canal (osteonic compact bone) (Figures 3 and 4). In the osteonic compact bone, the blood vessels and nerves travel through a channel known as Haversian canal. The Haversian system is composed of Haversian canal, concentric bone lamellae around the Harvesian canal, and osteocytes located among the lamellae. Haversian system is also known as osteon. Haversian canals of neighbor osteons are connected by transverse ducts referred as Volkmann canals. Usually, 4 to 20 bone lamellae are arranged around a Haversian channel. Osteocytes are located in small cavities, known as bone lacunae, within bone lamellae. From bone lacunae, small ducts or canaliculi are extended through the bone lamella. Osteocyte cellular processes are inside these small channels. Canaliculi make a net of channels that connect osteocytes with the Haversian canal. In this way, osteocytes may be fed by blood vessels.
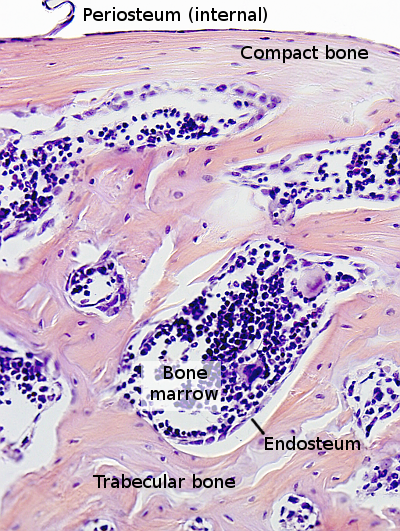
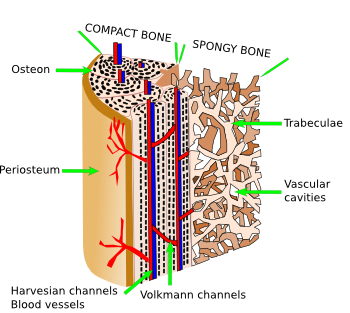
The inner surfaces of compact bone and vascular cavities of spongy bone are covered by connective tissue, the endosteum (Figure 3), which contains osteogenic cells, osteoblasts, and osteoclasts. Externally, the bone is covered by periosteum, which is formed by an outer layer of fibrous connective tissue and a inner layer containing osteogenic cells, where osteoblasts are found. Periosteum is attached to the bone by collagen bundles embedded in the calcified bone matrix.
4. Osteogenesis
Osteogenesis is the process of bone formation. It should be discerned between the origin of bone cells and the way the bone is formed. There are three cell lineages in the embryo that can differentiate into bone cells: paraxial mesoderm provides vertebrae and part of the skull and bones of the face, lateral mesoderm cells differentiate into the bones of the limbs, and neural crest cells, derived from ectoderm, differentiate into some bones of the skull and face. There are two ways for bone formation from mesenchymal cells (coming from some of the three lineages mentioned before): intramembranous and endochondral ossification. Intramembranous ossification is the formation of bone directly from mesenchymal cells, whereas during endochondral ossification there is first a differentiation of mesenchymal cells into cartilage, which is later substituted by bone tissue. As it can be noticed, bone tissue replaces a previous one in both differentiation processes. The first signal of bone tissue formation is the synthesis of a net of bone trabeculae, which are progressively remodeled as bone tissue matures.
Intramembranous ossification
In this type of ossification, mesenchymal cells are differentiated directly into bone cells (Figure 5). This process happens in flat bones. First, there is a condensation of mesenchymal cells in the place where the bone is going to be formed, and then there are strips of extracellular matrix organized as a reticular net. Some mesenchymal cells gather around these new strips and differentiate into osteoblasts, which start to synthesize bone extracellular matrix. A nucleation zone of ossification is generated, and the process of maturation of mesenchymal cells into osteoblasts is repeated at the border, so that the trabeculae grow. The extracellular matrix is secreted around osteoblasts, which become completely surrounded by bone matrix. Then, osteblasts differentiate into osteocytes. Periosteum is formed at the outer surfaces of this trabecular system, whereas endosteum appears at the surfaces of the internal cavities. Bone marrow develops in the internal space of these cavities.
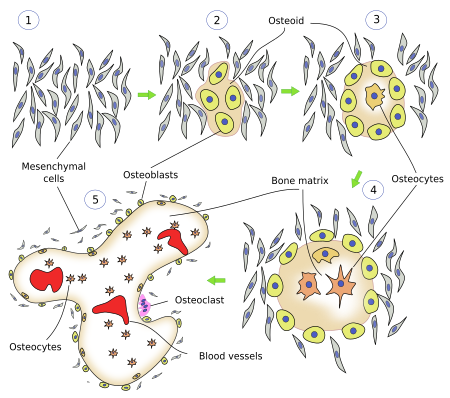
The organization of the initial bone matrix is referred as immature or reticular. By constant remodeling of the bone matrix, the reticular organization is transformed into a layered organization. Bones originated by intramembranous ossification do not develop typical osteones. They have compact bone in the periphery and cancellous bone in the inner parts.
Endochondral ossification
In this type of ossification, mesenchymal cells differentiate first into chondrocytes, which are later replaced by bone cells (Figure 6). After a compaction process, chondrocytes proliferate to form cartilage, which will be the scaffold to build the bone. At this time of development, some chondrocytes of the medial region stop proliferation. Then, chondrocytes grow in size and become hypertrophic chondrocytes. They synthesize a type of extracellular matrix containing molecules that favor the formation of minerals. Among the new molecules released to the extracellular matrix, there are two important for the formation of bone: an angiogenic that attract blood vessels toward the interior of the cartilage, and a molecule that makes the peripheral mesenchymal cells to differentiate into osteoblasts. Around the cartilage, a bone ring or bone collar is formed to support the new bone.
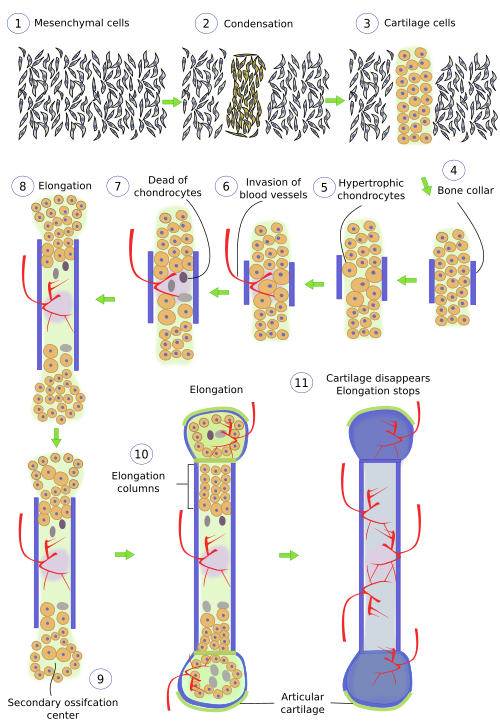
Hypertrophic chondrocytes die by apoptosis and the space left is invaded by blood vessels. Blood vessels invasion forms openings in the bone walls referred as nutrient foramens. Osteblasts enter the ossification area thanks to this blood vessels invasion and, as soon as they are inside, start to synthesize bone matrix. Meanwhile, osteoblasts that were differentiated in the old perichondrium also produce bone matrix that surrounds the degenerating cartilage. Periosteum progressively appears in this peripheral location. Internally, the area of dead chondrocytes expands along the cartilage structure, at the same time that it is being occupied by blood vessels that bring cells of the bone marrow, as well as osteoclasts. Osteoclasts differentiate from blood cells.
Some cartilage remains alive at the ends of long bones, allowing the growth in length of the bone during the juvenile stage of the animal. This cartilage disappears and ossifies when the animal enters adulthood. These remaining cartilage areas in young bones are known as physis or growth plates. There is a perichondral ring wrapping the growth plate, which allows the support and increase in diameter of this plate.
The diameter enlargement is possible because of the work of the periosteum, which produces bone by intramembranous ossification toward the inner part, and pushes itself outward.
 Cartilage
Cartilage 